
Diagnostic criteria:
2016 Fibromyalgia Diagnostic Criteria
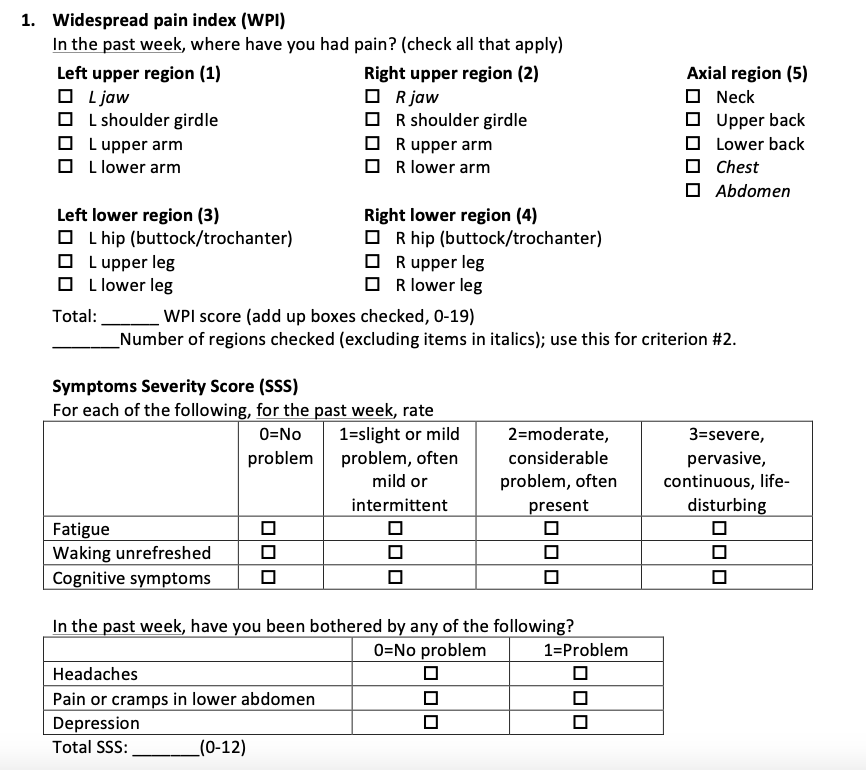
1. Widespread pain index (WPI) and symptom severity score (SSS)
- WPI≥7 and SSS≥5 OR WPI4-6 and SSS ≥ 9
2. Generalized pain: pain in 4/5 regions
3. Symptoms present ≥ 3 months
The fibromyalgia diagnosis can now be made irrespective of other diagnoses (you do not need to rule out all other conditions that could explain the symptoms, if criteria 1-3 are all met).
Presentation:
Chronic widespread pain, fatigue, sleep disturbances and also autonomic disturbances, cognitive dysfunction, hypersensitivity to external stimuli, somatic symptoms and psychiatric disorders.
Paraesthesia in the limbs, hands or trunk occurs in 20-30%
Fatigue is physical or mental. Degree of fatigue varies widely. Varied types of insomnia or frequent awakening is common. Sleep is non-restorative.
Cognitive dysfunction ('fibro-fog’) and memory deficits can be distressing
Mood - Depression, anxiety, pain or sleep problems can have a negative effect on cognitive symptoms but do not explain all cognitive symptoms
Headache with or without a history of migraine is very frequent
Gastric symptoms such as dyspepsia, abdominal pain and alternating constipation and diarrhoea are common
Genitourinary disorders (such as urinary urgency, dysmenorrhoea or vulvar vestibulitis) are frequent.
Morning stiffness occurs although does not usually exceed 60 min
Autonomic disturbances in all body areas and correlate with severity
E.g. Dry mouth (xerostomia) and eyes (xerophthalmia), blurred vision and photophobia, and Raynaud syndrome.
Lower limb discomfort and a need to move their legs continuously (restless legs syndrome) in 30%
Often a feeling of instability especially after standing upright for prolonged periods
Psychologically a preponderant negative affect is common.
This state of psychological suffering can accompany full-blown psychiatric disorders, which are frequent in patients with fibromyalgia and can notably affect the lives of the patients and even the severity of the syndrome.
The lifetime prevalence of anxiety disorders in patients with fibromyalgia is 60%, and depression is observed in 14–36% of patients compared with 6.6% of healthy individuals.
Suicide was ten times higher than in the general population
Depressive symptoms are NOT reported more frequently for patients with fibromyalgia than for patients with other painful conditions such as rheumatoid arthritis or cancer, and might be related to maladaptive coping with psychological distress.
Working activities, co-morbidities (such as obesity), and variations in temperature, modify symptom presentations. Physical or mental stress worsens pain
The diagnosis of fibromyalgia is exquisitely clinical.
Physical examination is not diagnostically useful because of its poor validity and poor reproducibility BUT is essential to rule out other diseases
Fibromyalgia has no pathognomonic feature, and so diagnostic clues have to be collected by means of thorough history taking.
The Simple Fibromyalgia Screening Questionnaire was also validated as a useful screening tool in 2019.
Epidemiology
Fibromyalgia is the third most frequent musculoskeletal condition (affecting 2-3% of the population), and its prevalence increases with age.
Poor quality of life of patients with fibromyalgia is reflected by massive health-care costs
The annual number of consultations required is almost double that of healthy individuals, and total health-care costs are estimated to be three times higher for patients with fibromyalgia than for other individuals.
Indirect societal costs are also high, mainly because of lost working productivity. One study showed that 24.3% of the patients involved in the study stopped working 5 years after fibromyalgia onset
Assessment of fibromyalgia should be holistic and not only consider all of the symptoms experienced by patients but also alleviating or aggravating factors and the effect of fibromyalgia on everyday life, functional status and working ability.
Pathophysiology
Fibromyalgia pathogenesis is not fully understood; hypotheses state that genetic predisposition, stressful life events, peripheral (inflammatory) and central (cognitive–emotional) mechanisms interplay to create pain dysperception owing to neuromorphological modifications (‘nociplastic pain’)
The central sensitisation co-opts novel inputs to nociceptive pathways that do not usually drive them. Thus sensations that arise from normal mechanical activity or posture are able to induce alpha-beta fibre-mediated pain. This leads to allodynia and hyperalgesia.
Likely contributors include: Abnormalities of descending inhibitory pathways, neurotransmitter abnormalities (aberrant serotonin messaging can link anxiety and pain. Elevated glutamate has been found in the CSF of fibromyalgia patients). Central sensitisation (pain amplified in the spinal cord via spontaneous nerve activity, expanded receptive fields and augmented stimulus responses).
Risk Factors
Many factors contribute to the development of fibromyalgia in a unique manner: genetic predisposition, personal experiences, emotional–cognitive factors, the mind–body relationship and a biopsychological ability to cope with stress.
Examination
A physical examination only reveals greater sensitivity to pressure at some specific points (‘tender points’), although these regions tend to be more tender than other regions in most individuals, regardless of whether they have fibromyalgia
These tender points are NOT the same as trigger points from myofascial pain
(Fibromyalgia is a CENTRAL abnormal processing issue, whereas trigger points are peripheral locations of dysfunction)
Often patients have increased sensitivity to pressure, and heat and cold
Reduced mechanical pain threshold
Presence of tender points which may represent secondary hyperalgesia
Exaggerate pain summation (wind up) and prolonged decay of pain
Investigations
Treatment
Treatment should be multimodal and built on four pillars (patient education; fitness; pharmacotherapy; and psychotherapy); the approach should be individualized, symptom-based and stepwise, establishing shared goals with the patient.

Prognosis
Prevention, as well as very early fibromyalgia diagnosis, remains an elusive goal, mainly owing to the lack of established risk factors (see the section on hypothetical pathogenic mechanisms).
In addition, insufficient data are available on the effect of early diagnosis on clinical progression; nonetheless, early recognition could enable the commencement of non-pharmacological approaches, such as psychotherapy or physical reconditioning, at an early stage and prevent the need for pharmacological treatments, therefore limiting adverse effects.
Golden pearls
References / Articles / Resources
Piercarlo, V. (2020). Fibromyalgia: an update on clinical characteristics, aetiopathogenesis and treatment. Nature Reviews. Rheumatology, 16(11), 645–660. https://doi.org/10.1038/s41584-020-00506-w
https://www.practicalpainmanagement.com/pain/myofascial/fibromyalgia-neuropathic-pain-disorder-link-small-fiber-neuropathy
Comments